Abstract
Background
Thrombosis is a common complication of myeloproliferative neoplasm (MPN) and its major cause of disability and death. With the development of next-generation gene sequencing technology, the relationship between non-driver mutations and thrombotic risk factors has also attracted close attention.
Methods
The clinical data of 125 MPN patients (75 ET and 50 PV) attending Xiyuan Hospital of the China Academy of Chinese Medical Sciences between January 2018 and March 2022 were retrospectively analyzed. A multivariate analysis of risk factors for thrombosis was performed using a Cox proportional hazards model.
Results
A total of 125 patients with MPN (75 ET and 50 PV) were evaluated, with a median age at diagnosis of 50 (18-78) years, 67 (53.6%) males and 58 (46.4%) females. The mutation rates of driver genes JAK2V617F, CALR, and MPL were 70.4%, 12.8%, and 0.8%, respectively. At least one non-driver mutation was detected in 36% of patients, with the highest rate of mutations in TET2 (12%), followed by ASXL1 (9.6%).
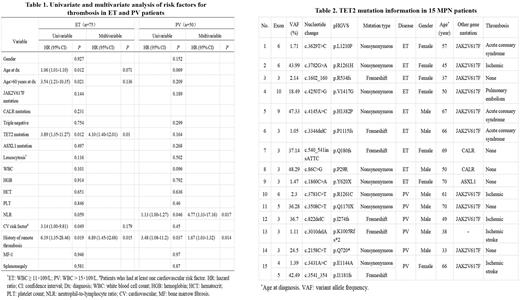
Thrombotic events occurred in 35 of 125 patients (28.0%), and the incidence of thrombotic events was 21.3% (16/75) in ET patients and 38.0% (19/50) in PV patients, respectively. For 125 MPN patients, univariate analysis revealed significant associations between thrombosis and age at diagnosis, age >60 years at diagnosis, JAK2V617F mutation, TET2 mutation, WBC, NLR, cardiovascular risk factors and history of remote thrombosis. In the multivariate analysis that included the above 8 factors as covariates, age at diagnosis (HR: 1.03, 95% CI: 1.00-1.06; P = 0.046), TET2 mutation (HR: 2.84, 95% CI: 1.26-6.36; P = 0.011), NLR (HR: 1.18, 95% CI: 1.06-1.32; P = 0.003), and history of remote thrombosis (HR: 5.33, 95% CI: 1.93-14.70; P = 0.001) remained risk factors for thrombosis in MPN patients. In the subgroup analysis of ET and PV patients, univariate analysis was performed for the parameters, and factors with differences were used as covariates for further multivariate analysis. In ET patients, multivariate analysis showed that TET2 mutation and a history of remote thrombosis were independent risk factors for thrombosis in ET patients, with an HR of 4.1 (95% CI: 1.40-12.01; P = 0.01) for TET2 mutation and 6.89 (95% CI: 1.45-32.68; P = 0.015) for history of remote thrombosis (Table 1). In PV patients, multivariate analysis observed neutrophil-to-lymphocyte ratio (NLR) (HR: 4.77, 95% CI: 1.33-17.16; P = 0.017) and a history of remote thrombosis (HR: 1.67, 95% CI: 1.03-1.32; P = 0.014) as independent risk factors for thrombosis, however, no association of TET2 mutation with thrombosis was observed in PV (Table 1).
Among 125 patients, TET2 mutations were detected in 15 patients (9 ET and 6 PV), with a mutation rate of 12%. Among them, 11 patients combined with JAK2V617F mutation (6 ET and 5 PV), 2 ET patients combined with CALR mutation and 1 ET patient combined with ASXL1 mutation. Two loci mutations of TET2 were detected in one patient with PV. The details of the 15 MPN patients with TET2 mutation are shown in Table 2.
Our study above have shown that TET2 mutation is an independent risk factor for thrombosis in ET patients, and to understand their clinical characteristics and coagulation status, we compared the clinical characteristics and coagulation function of TET2 mutated and unmutated patients. We found that the age of ET patients with TET2 mutation was significantly higher than that of patients without TET2 mutation (P < 0.05) . In terms of coagulation function, compared with ET patients without TET2 mutation, patients with TET2 mutation were in a relatively hypercoagulable state, as evidenced by a significant increase in D-Dimer (P < 0.01) and a significant decrease in antithrombin Ⅲ (AT-III) (P < 0.05).
Conclusion
TET2 mutation is an independent risk factor for thrombosis in ET patients, but no such association was observed in PV. Therefore, TET2 mutation is more valuable in predicting thrombosis in ET patients compared to PV. ET patients with TET2 mutation were older and in a relatively hypercoagulable state of coagulation compared to TET2 unmutated patients. However, prospective studies with more patients are needed to validate our results and to fully elucidate the association. Our study reports risk factors for thrombosis in MPN patients in Asia and complements the data on the relationship between non-driver mutations and thrombotic events in Asian MPN patients, providing a reference for future larger studies.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.